Cancer in Children: An Overview
Your child has been diagnosed with cancer. You are likely feeling shocked and scared. These feelings are normal, but remember you are not alone. Support and treatment are available. Your child’s healthcare team will help you and your child every step of the way.
What is cancer?
Cancer is a disease in which the body’s cells grow abnormally. Normally, cells grow at a steady rate. But with cancer, the cells grow out of control and crowd out normal cells. Cancer can start in any part of the body, such as the brain, muscles, bones, and blood cells.
With some cancers, the cells join together and form a lump of tissue called a tumor:
-
Malignant tumors. These tumors often grow fast and destroy healthy tissue. Malignant tumors can be metastatic. This means they can spread to other areas of the body.
-
Benign tumors. These are tumors that are not cancer. Benign tumors may be locally invasive. This means they don’t spread and affect only 1 part of the body. But they may still need treatment.
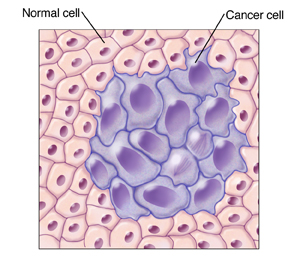 |
| Cancer occurs when normal cells begin to grow abnormally. |
-
Blood cancers (hematologic) are another type of cancer. They include leukemias and lymphomas.
What causes cancer?
Unlike cancer in adults, the cause of cancer in children is often not known. Parents of children with cancer often blame themselves. But cancer in children is no one’s fault. Changes in certain genes, called mutations, may affect the way your child’s cells grow. This gene mutation is random and couldn’t have been prevented. In rare cases, other factors play a role. These include exposure to certain viruses, chemicals, or radiation. It is very rare that cancer in children may be hereditary and may be more likely to happen in certain families.
What are the symptoms of cancer?
There is no single set of symptoms for cancer. Instead, your child’s symptoms depend on what type of cancer it is, the size of the tumor, and where the cancer is found.
How is cancer diagnosed?
Your child may have had a number of imaging or blood tests to diagnose cancer. More tests still may be needed. Often a biopsy, a small tissue sample of the tumor, may be removed and checked under a microscope in a lab. Your healthcare team can tell you more about any tests your child needs.
What is staging and grading?
Staging is the process that tells how big the cancer is and how much it has spread. Most cancers have their own staging system. Grading is used to describe how abnormal the cancer cells look when seen through a microscope. The more abnormal the cells are, the faster they grow. Staging and grading help the healthcare team plan treatment for your child. They also help determine the likelihood of a cure (prognosis). Staging and grading systems may look at the following:
-
Where the primary tumor is
-
How big the tumor is and how many there are
-
If the cancer has spread to other areas of the body (metastasis)
-
How abnormal the cancer cells look under a microscope
For many cancers, the stages are written as Roman numerals and can have a value of I through IV (1 through 4). The stage numbers refer to how big the tumor is and how much it has spread. For instance, stage I is an early stage of cancer. It means the cancer has not spread to other parts of the body. A stage IV cancer is the most widespread. Many cancers are broken down into further classifications. Your healthcare provider can tell you more if needed and answer any questions you have about the stage of your child’s cancer.
How is cancer treated?
Childhood cancers are often more curable than cancer in adults. The goal of treatment is to attack the abnormal cells, while damaging as few of the healthy cells as possible. To treat the cancer, your child may need more than one therapy. These may include the following:
-
Chemotherapy. Chemo kills cancer cells or shrinks tumors using strong medicine. This treatment often needs several sessions and has side effects. These side effects can include tiredness, hair loss, nausea, and vomiting. There are medicines available to help treat certain side effects.
-
Surgery. This removes all or part of a tumor.
-
Radiation. This kills cancer cells or shrinks tumors using high-energy waves, such as X-ray.
-
Targeted therapy. This works mostly on certain changes in the cancer cells and not on normal cells.
-
Immunotherapy. This can help your child's own immune system fight cancer.
-
Stem cell transplant. This can be used for leukemias and other cancers. It includes high-dose chemotherapy (and sometimes radiation therapy) to kill cancer cells. The stem cells are given after cancer treatment. This is done to help the bone marrow recover and start making blood cells.
It’s important that you follow your child’s treatment schedule as directed. Be sure to keep all your child’s healthcare appointments.
What is the likely outcome for my child?
The likelihood of cure may depend on the following:
-
The presence of symptoms related to the type of cancer
-
Type and stage of the cancer
-
Size and location of the tumor (if a tumor is present)
-
The look of the cancer cells under a microscope
-
If the cancer has spread
-
The child’s age and overall health
-
The cancer’s response to treatment
-
Your child's response to medicines, procedures, or therapies
Coping
You’re likely feeling many emotions right now. This is normal. Remember that you are not alone. Your child’s healthcare team will work with you and your child throughout your child’s illness and care. You may also want to get information and support for yourself. Learning about and talking with others who also have a child with cancer may help you and your family cope with the changes cancer brings. Some helpful resources are: