Having Endovascular Repair of an Abdominal Aortic Aneurysm (AAA)
Endovascular repair is a type of treatment for an abdominal aortic aneurysm (AAA). An AAA is a bulge in the wall of the large artery below your heart. The large artery is called the aorta. The bulge is caused by a weak section in the artery wall. The bulge is at risk of tearing. During the procedure, the weak section of the aorta is treated to stop it from tearing. Smaller, stable AAAs can be watched over time and treated with lifestyle changes and medicines. Other AAAs may require open abdominal surgery, which is more extensive than the endovascular repair.
What to tell your healthcare provider
Tell your healthcare provider about all the medicines you take. This includes over-the-counter medicines, herbs, and supplements. Let your provider know if you’ve ever had a problem with sedation or anesthesia. Also tell them if you are pregnant or think you might be pregnant. Tell your provider about any recent changes in your health, such as a fever.
Tests before your procedure
You may need some tests before your procedure, such as:
-
Blood tests to check for anemia and infection
-
An electrocardiogram (ECG), to check your heart rhythm
-
Ultrasound, to look at the size of your aneurysm
-
CT scan, to make detailed pictures of your aneurysm
-
Angiography, to get more information about your aneurysm
Getting ready for your procedure
Talk with your healthcare provider about how to get ready for your surgery. You may need to stop taking some medicines, such as blood thinners ahead of time. If you smoke, you’ll need to stop before your surgery. Smoking can delay healing. Talk with your healthcare provider if you need help to stop smoking. Follow any directions from your healthcare provider about not eating or drinking before your surgery.
On the day of your procedure
Endovascular repair is a minimally invasive procedure. This means it's done with a small cut (incision). A vascular specialist, such as a vascular surgeon, interventional radiologist, or an interventional cardiologist along with a team of specialized healthcare providers will do the surgery. Your healthcare provider can explain what to expect for your surgery. This is an example of how it is done:
-
You will likely be given general anesthesia. This prevents pain and causes you to sleep through the procedure.
-
A healthcare provider will carefully watch your vital signs, like your heart rate and blood pressure, during the procedure.
-
The surgeon will make a small cut in your groin and into an artery there. They will then insert a thin, flexible tube (catheter) into the artery.
-
The surgeon will gently guide the tube all the way to the aneurysm. The surgeon will use moving X-ray pictures to get to the right spot.
-
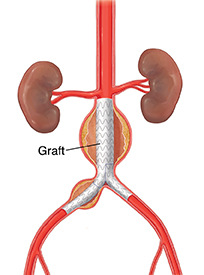
A stent graft is sent along the catheter to the aneurysm. The stent is a tube made of a thin metal mesh (the stent), covered with a thin polyester fabric (graft). The tube is collapsed so it's narrow and can fit through your blood vessel.
-
When the stent reaches the aorta, the surgeon will open it up and fasten it in place. The stent then stays in place, and blood flows through it. It protects that part of the aorta, and prevents the aneurysm from bursting.
-
Your surgeon will remove the catheter, close the incision, and put a small bandage on the wound.
After your procedure
After the procedure, you will spend several hours in a recovery room. Your healthcare team will closely keep track of your vital signs, such as your heart rate, blood pressure, and breathing. To help prevent bleeding, you may need to lie flat for several hours after the procedure. You may need to stay at the hospital for a day or more, depending on your condition. Your healthcare provider will tell you more about what to expect.
You may have some pain after the procedure. You can take pain medicine as advised by your healthcare provider. You can eat a normal diet as soon as you are able.
Recovering at home
You may need to take it easy for a little while after you get home. Ask your healthcare provider if you need to limit your activities. You may need to take medicines to help prevent blood clots.
Follow-up care
Follow up with your healthcare provider, or as advised.
When to call your healthcare provider
Call your healthcare provider right away if any of the following occur:
-
Fever of 100.4°F (38.0°C) or higher, or as directed by your healthcare provider
-
Symptoms that don’t get better
-
Pain that is getting worse
-
Infection at the incision site
-
Shortness of breath
-
New symptoms